สาเหตุของโรคอ้วน
ในปัจจุบันวิถีชีวิต และการรับประทานอาหารของคนไทยเปลี่ยนไปจากเมื่อก่อน เนื่องจากรูปแบบการใช้ชีวิตประจำวันของคนในปัจจุบันนั้นจะมีการใช้ชีวิตที่เร่งรีบ และต้องทำงานแข่งกับเวลาอยู่เสมอ ทำให้อาหารที่รับประทานเป็นอาหารแบบง่ายๆ ที่สะดวกและรวดเร็ว จากร้านสะดวกซื้อ หรือร้านอาหารที่เป็นแบรนด์จากต่างชาติ (Fast Food) ทำให้คุณค่าทางอาหารที่ได้รับต่ำ เพราะอาหารเหล่านี้จะเป็นอาหารจำพวกแป้ง และไขมัน มีการรับประทานผักและผลไม้น้อยลง ความเร่งรีบในการทำงาน ทำให้โอกาสในการออกกำลังกายมีน้อยลง คนไทยจึงเป็นโรคอ้วนกันเยอะมากขึ้น มีรูปร่างอุ้ยอ้าย อึดอัด และมีโรคอื่น ๆ คุกคามแทรกซ้อน ได้แก่ โรคเบาหวาน ความดันโลหิตสูง โรคหัวใจ และไขมันในหลอดเลือดสูง มีความเสี่ยงในการเสี่ยงในการเป็น อัมพฤกษ์ อัมพาต ทำให้อายุสั้นกว่าคนทั่วไป
นอกจากนี้ ความผิดปกติของระดับ Gut Hormone ในกระเพาะอาหาร จะมีผลต่อความหิว ความอิ่มและระดับน้ำตาลในเลือด
วิธีการวัดความอ้วนของร่างกาย
ความอ้วนนั้นสามารถคาดคะเนจากสายตาแล้ว อาจจะใช้วิธีวัดความอ้วน โดยการคำนวนดัชนีมวลกาย หรือ Body Mass Index (BMI) เป็นค่าดัชนีที่คำนวณจากน้ำหนักและส่วนสูง เพื่อใช้เปรียบเทียบความสมดุลระหว่างน้ำหนักตัวต่อความสูง เพื่อวัดความอ้วน-ผอม สามารถคำนวนได้โดยนำน้ำหนักตัว (กิโลกรัม) หารด้วยกำลังสองของส่วนสูงตนเอง (เมตร) โดยเมื่อคำนวนแล้วสามารถนำมาเปรียบเทียบเกณฑ์ได้ดังนี้
- ผอมเกินไป: น้อยกว่า 18.5 (<18.5)
- เหมาะสม: มากกว่าหรือเท่ากับ 18.5 แต่น้อยกว่า 25 (≥18.5 แต่ <25)
- น้ำหนักเกิน: มากกว่าหรือเท่ากับ 25 แต่น้อยกว่า 30 (≥25 แต่ <30)
- อ้วน: มากกว่าหรือเท่ากับ 30 แต่น้อยกว่า 40 (≥30 แต่ <40)
- อันตรายมาก: มากกว่าหรือเท่ากับ 40 (≥40)
(http://th.wikipedia.org/wiki/ดัชนีมวลกาย)
( BMI Calculator )
แนวทางการรักษาโรคอ้วน

1. การควบคุมอาหารควบคู่กับการออกกำลังกาย
เป็นการรักษาโรคอ้วนที่ได้ผลและปลอดภัยมากที่สุด โดยควรรับประทานอาหารที่มีประโยชน์ เน้นอาหารจำพวกโปรตีน ผัก ผลไม้ และอาหารที่มีวิตามินสูง ลดอาหารจำพวกแป้ง ไขมัน และน้ำตาล ขณะเดียวกันควรออกกำลังกายเพื่อควบคุมน้ำหนัก โดยควรออกกำลังกายเป็นประจำอย่างน้อย 4 ครั้ง/สัปดาห์ และในการออกกำลังกายแต่ละครั้งไม่ควรต่ำกว่า 30 นาที โดยเน้นการออกกำลังกายแบบคาร์ดิโอ (Cardio) เช่น วิ่ง ปั่นจักรยาน ว่ายน้ำ เป็นต้น ซึ่งเป็นการออกกำลังที่ช่วยในการเผาผลาญไขมันได้เป็นอย่างดี หากหลังจากการควบคุมอาหารและออกกำลังกายแล้วน้ำหนักยังขึ้นอยู่ รวมถึงมีปัจจัยเสี่ยงของโรคต่าง ๆ หรือมี BMI สูงเกิน 25 แต่ไม่มีปัจจัยเสี่ยงร่วมด้วย แพทย์อาจจะพิจารณาให้ยารักษาโรคอ้วน ถ้าหากรักษาด้วยยาแล้ว BMI ยังสูงเกิน 30 และมีปัจจัยเสี่ยงของโรคร่วมด้วย อาจจะต้องรักษาด้วยการผ่าตัด
2. การรักษาด้วยยา
การรักษาด้วยยานั้น ยาจะมีผลต่อจิตประสาท เป็นยาที่ไม่ควรซื้อมารับประทานเอง จึงควรอยู่ภายใต้การดูแลของแพทย์อย่างเคร่งครัด ขณะเดียวกันการรักษาด้วยยา ควรจะควบคู่กับการควบคุมอาหารและออกกำลังกายด้วย โดยผู้ที่ควรได้รับการรักษาโรคอ้วนด้วยยานั้น จะต้องมี BMI มากกว่าหรือเท่ากับ 30 หรือ ผู้ที่มี BMI มากกว่าหรือเท่ากับ 27 และมีปัจจัยเสี่ยงร่วมด้วย
3. การผ่าตัดรักษาโรคอ้วน (Bariatric Surgery)
เป็นการลดขนาดของกระเพาะอาหารเป็นการตัดกระเพาะอาหารให้เล็กลงทำให้ฮอร์โมน Gut Hormone ต่างๆลดลง ทำให้ไม่รู้สึกหิว (ทานนิดเดียว จะรู้สึกอิ่มไว) จึงปลอดภัยกว่า ควบคุมการหิวได้ดีกว่า
การผ่าตัดลดน้ำหนักรักษาโรคอ้วนมีหลายวิธี ดังนี้
1.การใส่บอลลูน (Gastric Balloon )
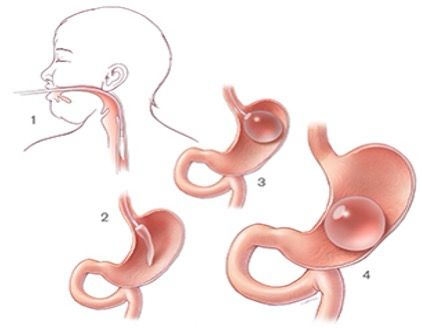
รูปที่ 1 : การใส่บอลลูน Gastric Balloon
Gastric balloon คือ การใส่บอลลูนที่บรรจุสารน้ำเข้าไปในกระเพาะอาหาร โดยบอลลูนจะเข้าไปลดความจุของกระเพาะอาหารทำให้รับประทานอาหารได้น้อยลงอิ่มนานกว่าเดิม ร่างกายจะมีการดึงเอาไขมันที่สะสมไว้ มาใช้ เป็นพลังงานแทน ทำให้ลดน้ำหนักอย่างปลอดภัย การทำ Gastric balloon เหมาะสมกับ ผู้มี BMI ประมาณ 27-30
ขั้นตอนการทำ Gastric balloon
บอลลูนจะถูกใส่เข้าไปทางปากด้วยเทคนิคการส่องกล้อง ไม่มีแผลผ่าตัด บอลลูนทำจากวัสดุซิลิโคนทางการแพทย์ ฉีดสารน้ำเข้าไปในบอลลูน ประมาณ 400-500 ซีซี แต่สามารถปรับขนาดขึ้นอยู่กับขนาดของกระเพาะ ประมาณ 6-12 เดือน เมื่อน้ำหนักลดได้ที่แล้ว ก็จะเอาออก
หลังผ่าตัด 2-5 วัน อาจจะมีอาการ คลื่นไส้อาเจียน รู้สึกไม่สบายตัว ปวดท้องเกร็ง หลังใส่บอลลูน 3-4 สัปดาห์ สามารถรับประทานอาหารปกติได้ สามารถออกกำลังกายได้ปกติ
ข้อดีของการทำ Gastric balloon
- ่เป็นการลดน้ำหนักที่มีความเสี่ยงต่ำ ผลข้างเคียงน้อยเมื่อเทียบกับการผ่าตัดลดน้ำหนักวิธีอื่นๆ
- ไม่มีแผลผ่าตัด
- สามารถเพิ่ม หรือลดขนาดบอลลูน ได้ตามต้องการ
- อาจจะทำซ้ำได้ หากน้ำหนักตัวเพิ่มขึ้นมาอีก
ข้อควรปฏิบัติ หลังการใส่บอลลูน
- หลังการใส่บอลลูนไม่ควรดื่มน้ำแต่ละครั้งมากเกิน ครึ่งแก้ว ควรดื่มบ่อยๆทุก 1-2 ชั่วโมง
- พบแพทย์ติดตามอาการตามนัดทุกครั้ง
- รับประทานยา ป้องกัน แผลในกระเพาะ ลดความเสี่ยงของการเกิดแผลในกระเพาะ
- หลีกเลี่ยงการใช้ยาแก้ปวดแบบสเตียรอยด์ งดการดื่มแอลกอฮอล์ ลดความเสี่ยงของการเกิดแผลในกระเพาะ
- เมื่อรู้สึกผิดปกติ ควรรีบมาพบแพทย์ทันที
- เมื่อครบกำหนดเอาบอลลูนออก ต้องปรับเปลี่ยนพฤติกรรม เพื่อรักษาน้ำหนัก
หลักการรับประทานอาหาร หลังการใส่บอลลูน
- สองอาทิตย์แรก รับประทานอาหารอ่อน ย่อยง่าย
- รับประทานอาหารที่มีประโยชน์ ทางโภชนาการ
- ค่อยๆเพิ่มอาหาร ถ้ามีอาการเจ็บ หรืออึดอัด ควรหยุดและ เริ่มใหม่
- เพิ่มปริมาณอาหาร เคี้ยวอาหารช้าๆใช้เวลารับประทานอาหารมากขึ้น
- หลีกเลี่ยงน้ำหวาน หรือน้ำผลไม้
- รับประทานอาหารที่มีโปรตีนทุกมื้อ
- การที่มีแรงดันอาหาร ออกมา เป็นเพราะ รับประทานอาหาร มากไป หรือเร็วไป ควรหยุดพัก 10-15 นาที และครั้งต่อไป ให้รับประทานน้อยลงและช้าลง
2.การผ่าตัดรัดกระเพาะอาหาร (Gastric ฺBanding )
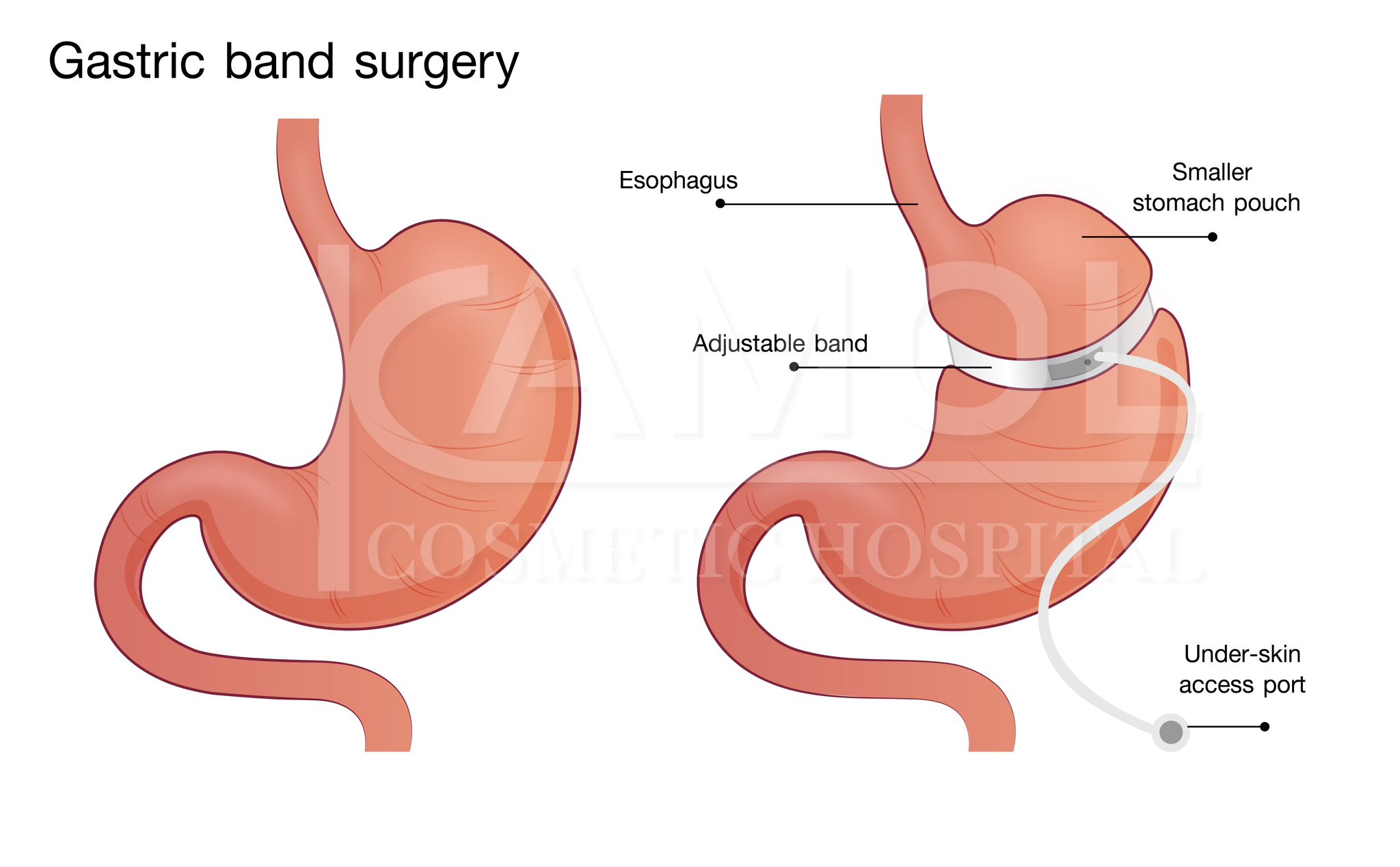
รูปที่ 2 : การตัดกระเพาะด้วยสายรัดกระเพาะ Gastric Band
เป็นสายรัดที่สามารถปรับขนาดการรัดขนาดกระเพาะ ทำให้กระเพาะเล็กลง ไปลดความจุของกระเพาะอาหารทำให้รับประทานอาหารได้น้อยลง ร่างกายจะมีการดึงเอาไขมันที่สะสมไว้ มาใช้ เป็นพลังงานแทน ทำให้ลดน้ำหนักอย่างปลอดภัย การทำ Gastric balloon เหมาะสมกับ ผู้มี BMI ประมาณ 30 เป็นการผ่าตัดด้วยการส่องกล่อง
ขั้นตอนในการลดน้ำหนักด้วยสายรัดกระเพาะ Gastric Band
- ผ่าตัดด้วยการส่งกล้อง ภายใต้การดมยาสลบ
- ใส่ Gastric band รัดกระเพาะด้านบน ปรับความตึงให้พอเหมาะกับแรงดันของกระเพาะ หลังใส่ แก๊ส คาร์บอนไดออกไซด์
- การผ่าตัดใช้เวลา 30-60 นาที
- วิธีการรับประทานอาหาร หลังการผ่าตัดรัดกระเพาะ เหมือนกับการ ใส่บอลลูน
- สามารถใส่ไว้ ได้นาน เป็น 10 ปี สามารถ เอาออกได้
ผลข้างเคียงของการผ่าตัดรัดกระเพาะ Gastric Band
- หลอดอาหารอาจจะขยายใหญ่ขึ้น
- เป็นแผลในกระเพาะ และหลอด อาหาร
- ติดเชื้อ
- อาจจะเกิดการเลื่อนหลุดของสายรัดกระเพาะ
- การสึกกร่อนของสายรัดกระเพาะ
3.การผ่าตัดกระเพาะแบบตัดเนื้อกระเพาะออก (Vertical Sleeve Gastrectomy)
การผ่าตัดกระเพาะ แบบตัดเนื้อกระเพาะออก (Sleeve Gastrectomy) เป็นวิธีการตัดเอาเนื้อกระเพาะออกบางส่วน ตามแนวยาวจากบนลงล่าง (Verticle ) เพื่อลดขนาดกระเพาะอาหารให้เล็กลง เพื่อให้รับประทานได้น้อยลง สำหรับผู้ที่เป็นโรคอ้วน จะช่วยลดปริมาณอาหารที่รับประทานเข้าไป ซึ่งการตัดกระเพาะจะทำให้ผู้ที่ตัดกระเพาะไปแล้วนั้น สามารถประสบความสำเร็จในการลดน้ำหนัก มีน้ำหนักที่ลดลง จากการศึกษาพบว่า การผ่าตัดกระเพาะ แบบ Sleeve Gastrectomy ปลอดภัยกว่า ปัญหาแทรกซ้อนน้อยกว่าการทำ By pass. สามารถทำให้คนอ้วนที่มี โรคความดัน เบาหวาน หลังตัดกระเพาะจะมีอาการดีขึ้นอย่างชัดเจน
การผ่าตัดกระเพาะแบบตัดเอาเนื้อกระเพาะออก (Sleeve Gastrectomy) มีการผ่าตัด 2 เทคนิค
- ผ่าตัดกระเพาะอาหารแบบส่องกล้อง (Minimally invasive Sleeve Gastrectomy)
- ผ่าตัดกระเพาะอาหารแบบ เปิดแผลหน้าท้อง (Open Sleeve Gastrectomy) เป็นการผ่าตัดแบบเก่าที่จะเกิดแผลเป็นขนาดใหญ่ ปัจจุบันไม่นิยม
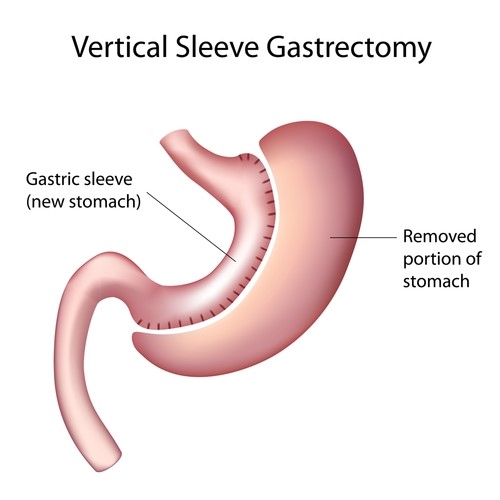
รูปที่ 3 : การตัดกระเพาะแบบเอาเนื้อกระเพาะออก Vertical Sleeve Gastrectomy
การผ่าตัดกระเพาะแบบ Vertical Sleeve Gastrectomy เป็นการผ่าตัดเอากระเพาะอาหารออกประมาณ 70-85 เปอร์เซ็นต์ กระเพาะอาหารที่เหลือจะลักษณะคล้ายกล้วย การผ่าตัดกระเพาะแบบ Sleeve Gastrectomy แตกต่างจากขั้นตอนการผ่าตัดลดความอ้วนด้วยวิธีอื่นๆ เนื่องจากการผ่าตัดวิธีนี้อาหารเข้าสู่กระเพาะอาหารใหม่ จากนั้นอาหารจะไปตามเส้นทางเดินอาหารเดิมปกติ จึงไม่มีปัญหาในการดูดซึม การผ่าตัดกระเพาะแบบ Sleeve Gastrectomy ทำให้ช่วยลดปริมาณอาหาร (และแคลอรี) ที่บริโภคได้ และยังส่งผลต่อฮอร์โมนในลำไส้ Gut Hormone ซึ่งส่งผลต่อหลายปัจจัยเช่นความหิว,ความอิ่ม และการควบคุมระดับน้ำตาลในเลือด การผ่าตัดกระเพาะอาหารยังช่วยควบคุมโรคเบาหวานประเภท 2 ได้อีกด้วย หลังผ่าตัดจะทำให้รู้สึกอิ่มเร็วและกินได้น้อยลง
ข้อดีของการผ่าตัดกระเพาะแบบ Minimal Invasive Sleeve Gastrectomy
-
ผ่าตัดด้วยกล้อง แผลเล็กมาก Minimal Invasive Surgery
-
ใช้เวลาพักฟื้นน้อยกว่า การผ่าตัดกระเพาะแบบอื่น ๆ เพียง 3-4 วัน ในโรงพยาบาล
-
กระเพาะอาหารมีขนาดเล็กลง รับประทานอาหารได้น้อยลง รู้สึกอิ่มเร็วขึ้น
-
เกิดการสลายไขมันอย่างรวดเร็ว ทำให้น้ำหนักตัวหายไปอย่างรวดเร็ว
-
ไม่มีสิ่งแปลกปลอมในกระเพาะเช่น Balloon หรือนอกกระเพาะ เช่น ตัวรัดกระเพาะ
-
ก่อให้เกิดการเปลี่ยนแปลงที่ดีของฮอร์โมนในลำไส้ Gut Hormone มีปริมาณน้อยลง ไม่ไปกระตุ้นการอยากอาหาร ไม่ค่อยหิว และเวลากินจะกินได้น้อยลง
ข้อเสียของการผ่าตัดกระเพาะแบบเอาเนื้อกระเพาะออก ด้วยการส่งกล้อง
-
เมื่อตัดกระเพาะแล้วจะไม่สามารถทำให้กระเพาะกลับมาเป็นเหมือนเดิมได้อีก
-
อาจทำให้เกิดการขาดวิตามิน หรือสารอาหารบางอย่าง ในระยะยาว
ขั้นตอนการผ่าตัดกระเพาะ
การผ่าตัดกระเพาะแบบ Sleeve Gastrectomy minimal invasive surgery จะผ่าตัดโดยการส่องกล้องใช้เวลาผ่าตัด 2-3 ชั่วโมง
- ดมยาสลบโดยวิสัญญีแพทย์
- ศัลยแพทย์จะทำการเปิดแผลเล็ก ๆ 4จุด บริเวณหน้าท้อง จากนั้นจะสอดกล้องขนาดเล็ก (laparoscope) และเครื่องมือเล็กๆ อื่นๆ เข้าไปในแผลเหล่านี้เพื่อผ่าตัดเอาส่วนหนึ่งของกระเพาะออกประมาณ 70 % ออกทางรูแผลที่เจาะไว้ และเย็บกระเพาะอาหาร จะทำให้ได้กระเพาะอาหารที่เล็กลง
- เย็บปิดแผลบริเวณหน้าท้อง 4 จุด

รูปที่ 3.1: แผลผ่าตัดกระเพาะ แบบ Minimal Invasive Sleeve Gastrectomy

รูปที่ 3.2: การผ่าตัดกระเพาะด้วยกล้อง Minimal Invasive Sleeve Gastrectomy

รูปที่ 3.3: กระเพาะอาหารที่ถูกตัดออกมา
4. การผ่าตัดกระเพาะอาหารแบบบายพาส(Gastric Bypass (Roux-en-Y gastric Bypass)
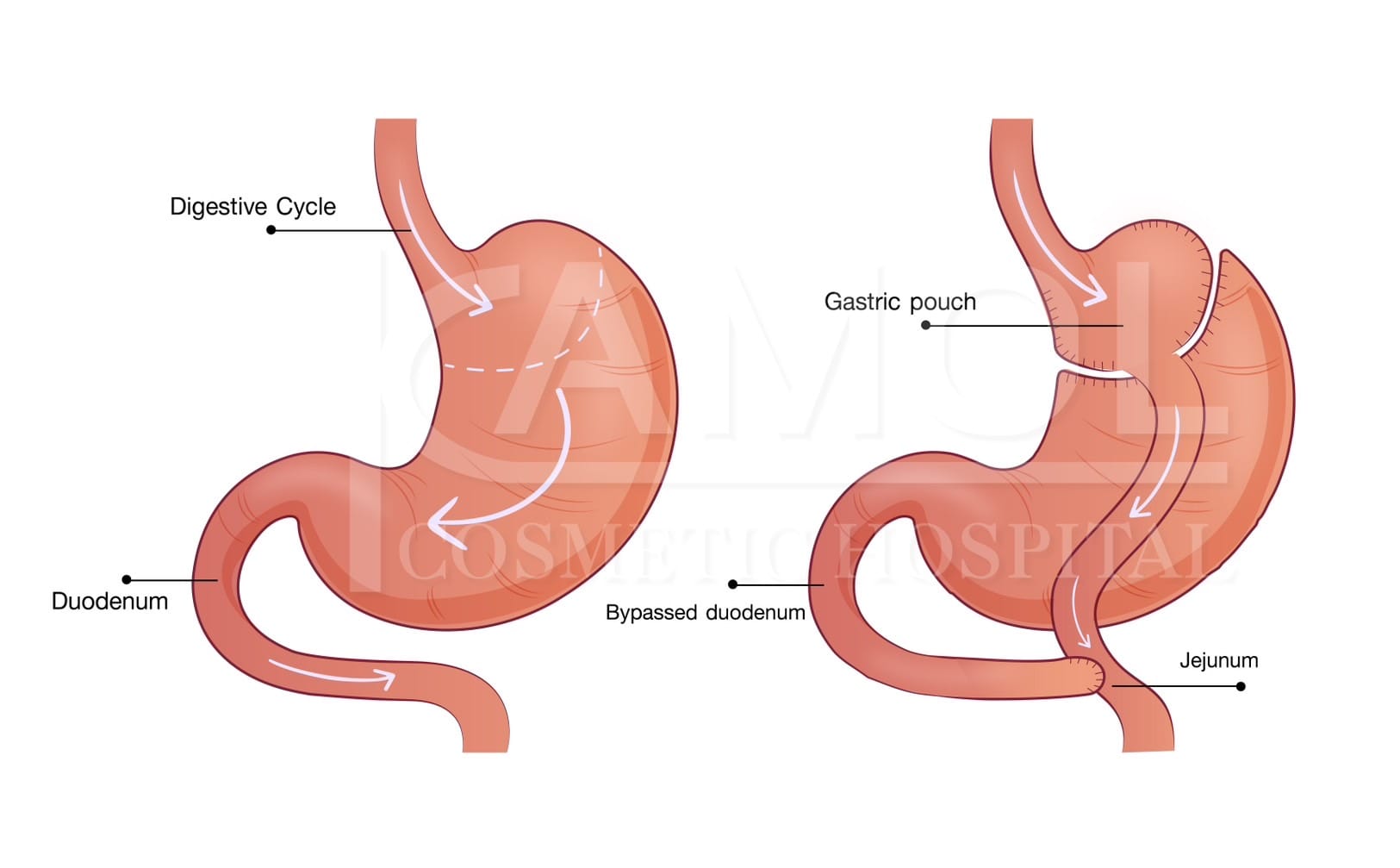
รูปที่ 4: การผ่าตัดกระเพาะอาหารแบบบายพาส(Gastric Bypass (Roux-en-Y gastric Bypass)
การผ่าตัดกระเพาะอาหารแบบ บายพาส คือการผ่าตัดกระเพาะเพื่อลดน้ำหนักแบบหนึ่ง โดยการเป็นการผ่าตัดแบ่ง กระเพาะlส่วนบนให้มีขนาดเท่า "ไข่ไก่" จากนั้นตัดลำไส้เล็กดึงขึ้นต่อเข้ากับกระเพาะอาหารเล็กๆ ที่ทำขึ้นใหม่ และ ในส่วนปลายของกระเพาะอาหารเดิมจะมีส่วนของลำไส้เล็กส่วนต้น Duodenum ต่อเข้ากับ ลำไส้เล็ก ส่วนกลาง หรือ ๋jejunum ที่ต่อมาจากกระเพาะอาหาร ใหม่ ขนาดเท่าไข่ไก่ อาหารที่รับประทานจะผ่านจากหลอดอาหาร เข้าสู่กระเพาะเล็กๆ แล้วเข้าสู่ลำไส้เล็ก เป็นการต่อตรงเข้า จากหลอดอาหารสู่ ลำไส้ น้ำย่อยจากกระเพาะ จะผสมกับอาหารเข้าสู่ลำไส้เล็ก จะถูกย่อยที่ลำไส้เล็ก ทางเดินอาหารจะสั้นลง
การผ่าตัดกระเพาะแบบ บายพาส หรือ แบบ Roux-en-Y เป็นการผ่าตัดลดน้ำหนักอีกแบบหนึ่ง โดยการสร้างกระเปาะขนาดเล็ก จากกระเพาะอาหารส่วนบน และเชื่อมต่อโดยตรงกับลำไส้เล็กดังรูป วิธีนี้อาหารจะผ่านข้ามกระเพาะอาหารส่วนใหญ่ไปยังลำไส้เล็กโดยตรงเลย ที่ลำไส้เล็กส่วนแรก ส่งผลให้ปริมาณอาหารที่สามารถบริโภคได้ลดลง และจำกัดการดูดซึมของสารอาหาร และวิตามิน
ข้อดีของการผ่าตัดกระเพาะแบบบายพาส (Gastric Bypass)
- มีประสิทธิภาพในการลดน้ำหนัก 60-80% ประสบความสำเร็จ น้ำหนักลดลงอย่างรวดเร็ว ภายใน 1-2 ปี
- ลดการปัญหาโรคที่เกิดจาก เบาหวาน ความดัน และ การหยุดหายใจเวลานอน Sleep apnea
- ,มีประสิทธิภาพในการลดน้ำหนักดีมาก และสามารถควบคุมน้ำหนักในระยะยาวได้ดี
ข้อเสียของการผ่าตัดกระเพาะแบบบายพาส (Gastric Bypass)
- การผ่าตัดกระเพาะแบบบายพาส จะมีความซับซ้อน การตัดเนื้อกระเพาะออก (sleeve gastrectomy) .ใช้เวลาผ่าตัดนานกว่า และพักฟื้นนานกว่า
- มีความเสี่ยงหลังการผ่าตัด สูงกว่า การตัดเนื้อกระเพาะออก (sleeve gastrectomy) เช่น การรั่ว การติดเชื้อ และ เลือดออก
- มีผลเสียต่อระบบการย่อยอาหาร และ การดูดซึม สารอาหาร และ วิตามิน เกลือแร่ ที่จำเป็นต่อร่างกาย
- อาจเกิด อาการ คลื่นไส้ อาเจียน ท้องเสีย หลังการผ่าตัด เนื่องจาก อาหารผ่านเข้าสู่ลำไล้เล็กอย่งรวดเร็ว
- ความสามารถในการรับประทานอาหารน้อยลงไปมากเพราะมีกระเพาะอาหารที่เล็กมาก ต่อตรงกับลำไส้เล็ก จึงไม่มีที่เก็บอาหารหลังรับประทาน ต้องจำกัดการรับประทานอาหารแต่ที่จำเป็นต่อร่างกายจริงๆเท่านั้น
ผู้ที่เหมาะสมกับการผ่าตัดกระเพาะ
- เป็นโรคอ้วน และมี BMI สูง มากกว่า 40 ขึ้นไป
- มี BMI ระหว่าง 30 - 40 แต่มีภาวะที่เกี่ยวข้องกับโรคอ้วน เช่นโรคเบาหวานประเภท 2 หรือความดันโลหิตสูง
- อายุไม่เกิน 65 ปี
- สุขภาพร่างกายแข็งแรงพอที่จะ ดมยาสลบได้
- เป็นคนอ้วน ที่เคยลดน้ำหนักวิธีต่างๆแล้วไม่ได้ผล เช่นการอดอาหาร การออกกำลังกาย หรือใช้ยา
- มีวินัยในการดูแลสุขภาพ ควบคุมการรับประทานอาหาร ปฏิบัติตามคำแนะนำของแพทย์และโภชนากร และ พบแพทย์ตามนัดทุกครั้ง
คนไข้ต้องมาปรึกษาแพทย์หากคุณคิดว่าการผ่าตัดลดน้ำหนักอาจเป็นทางเลือกที่ดีสำหรับคุณ หากคุณมีคุณสมบัติที่พร้อมสำหรับการรักษา เราสามารถแนะนำคุณเพื่อรับการประเมินเพื่อตรวจสอบในการผ่าตัดได้
ข้อดีของการผ่าตัดกระเพาะ
- ทานอาหารได้น้อยลง ประหยัดค่าใช้จ่าย
- มั่นใจในรูปร่างของตัวเอง
- ลดโรคที่เกิดจากโรคอ้วน
- ใส่เสื้อผ้าง่ายขึ้น มีความมั่นใจ
การเตรียมตัวก่อนผ่าตัดกระเพาะอาหาร
- คนไข้ต้องปรึกษาผู้เชี่ยวชาญก่อนทำการผ่าตัด ซึ่งประกอบด้วย
- นักโภชนบำบัด
- นักจิตวิทยา
- อายุรแพทย์ที่ชำนาญในการดูแลผู้ป่วยภาวะอ้วน
- ศัลยแพทย์ผู้เชี่ยวชาญด้านการทำผ่าตัดในผู้ป่วยภาวะอ้วน
การขอคำปรึกษา และการปฏิบัติตัว
- นักโภชนบำบัดจะอธิบายว่าควรทานอาหารมากน้อยแค่ไหนหลังทำการผ่าตัด และก่อนผ่าตัดจะต้องลดน้ำหนักเท่าไร
- นักจิตวิทยา ช่วยในเรื่องการลดความเครียดที่อาจมีมากขึ้นในช่วงก่อน-หลังผ่าตัด
- แพทย์อายุรกรรม จำเป็นต้องตรวจสุขภาพให้คำปรึกษาการรักษาเพิ่มเติม หรือให้คำปรึกษาทางยาในการลดน้ำหนักบ้างก่อนการผ่าตัด และดูแลโรคที่มาพร้อมกับความอ้วน
- แพทย์ผ่าตัด อธิบายถึงทางเลือกกับผู้ป่วยว่าการทำผ่าตัดแต่ละแบบมีข้อดี ข้อเสียอย่างไร เพื่อผู้ป่วยจะพิจารณาได้ว่าวิธีใดเหมาะสมกับตน
การดูแล หลังผ่าตัดกระเพาะ
-
อาจมีสายเดรน ระบายน้ำเล็ก ๆ เพื่อระบายของเหลวส่วนเกินออกไป
-
อาจมีสายสวนที่ระบายปัสสาวะออกจากกระเพาะปัสสาวะ
-
งดออกกำลังกายและยกของหนัก อย่างน้อย 1 เดือน
-
ตัดไหมหลังผ่าตัด 7 วัน
-
ทานอาหารเหลว ประมาณ 4-6 สัปดาห์ หลังการผ่าตัด
-
เมื่อคุณรับประทานอาหารได้ปกติ สิ่งสำคัญคือต้องทานอาหารที่มีประโยชน์ ต่อสุขภาพ เพื่อช่วยในการลดน้ำหนักอย่างต่อเนื่อง
-
กลับไปทำกิจกรรมตามปกติได้ภายใน 2-4 สัปดาห์หลังการผ่าตัดกระเพาะ
-
มาพบแพทย์ตามนัดทุกครั้ง
-
ออกกำลังกายเมื่อรู้สึกดีขึ้น มีโปรแกรมการออกกำลังกาย สำหรับผ่าตัดกระเพาะโดยเฉพาะ
-
ต้องเข้ามารับการดูแลเรื่องโภชนาการจากนักโภชนาต่อหลังผ่าตัด 1 เดือน
ความเสี่ยงและภาวะแทรกซ้อนที่อาจเกิดขึ้นได้หลังผ่าตัดกระเพาะ
-
มีเลือดออก
-
มีการติดเชื้อ
-
กระเพาะอาหารรั่ว (leakin bowels)
-
ต้องทำการผ่าตัดใหม่
-
ความเสี่ยงจากการดมยาสลบ
หลังผ่าตัด อาจมีภาวะแทรกซ้อนสำคัญที่อาจเกิดขึ้นได้ คือ อาจมีเลือดอุดตันที่เท้า ปอด หัวใจ, เกิดโรคปอดบวม, ทางเดินปัสสาวะอักเสบ คล้ายการทำผ่าตัดทั่วไป แต่ภาวะแทรกซ้อนอาจน้อยลงหากการทำผ่าตัดลดน้ำหนักทำในสถานพยาบาล/ศูนย์ที่มีแพทย์, ทีมที่เชี่ยวชาญ และมีเครื่องมือแพทย์พร้อม มีการติดตามผู้ป่วยหลังผ่าตัดสม่ำเสมอ โดยมีทีม รวมทั้งพยาบาลผู้ดูแลที่ได้รับการฝึกฝนในการดูแลผู้ป่วยประเภทนี้เป็นพิเศษ รวมทั้งแพทย์ดมยามีความเชี่ยวชาญในการดมยาผู้ป่วยอ้วนเป็นอย่างดี
ผลลัพธ์หลังการผ่าตัดกระเพาะ
ผลดีของการผ่าตัดกระเพาะ คือน้ำหนักลดอย่างรวดเร็ว ลดโรคที่เกี่ยวกับโรคอ้วน และอันตรายจากโรคอ้วนได้ ทำให้ร่างกายดูดี ลดค่าใช้จ่ายในการดูแลสุขภาพ เช่น โรคเบาหวาน ความดันโลหิตสูง นอนกรน ทำให้ใช้ยาลดน้ำหนักลดลงหรือไม่ต้องใช้ยาลดน้ำหนักอีก รวมถึงลดความเสี่ยงจากโรคหัวใจ มะเร็งได้
การรับประทานอาหารหลังการผ่าตัดกระเพาะอาหาร
1-7 วัน หลังการผ่าตัด
รับประทานอาหารเหลว หรือเครื่องดื่มที่มีลักษณะเหลวใส ไม่มีกากใย ไม่มีแก๊ส และไม่ใส่น้ำตาล
-
น้ำสมุนไพร (ไม่ใส่น้ำตาล)
-
น้ำซุปใส
-
น้ำผลไม้ที่ผ่านการกรองกากใย และไม่ใส่น้ำตาล
1 สัปดาห์ หลังการผ่าตัด
เริ่มทานอาหาร หรือเครื่องดื่มที่มีเนื้อ หรือมีความข้นเพิ่มมากขึ้นได้ แต่ต้องมีโปรตีนสูง ไขมันต่ำ และไม่มีกากใย รวมถึงไม่ใส่น้ำตาล
-
ซุปข้น
-
นมจืด หรือนมพร่องมันเนย
-
น้ำเต้าหู้ ไม่ใส่น้ำตาล
-
โยเกิร์ตรสธรรมชาติ
2 สัปดาห์ หลังการผ่าตัด
เริ่มรับประทานอาหารอ่อน หรือย่อยง่าย คล้ายกับอาหารเด็กได้แล้ว
-
ไข่ตุ๋นหมูบด
-
ปลานึ่ง
-
เกี๊ยวน้ำ
-
แกงจืดเต้าหู้ไข่
-
ข้าวต้มปลา
-
โจ๊กหมูบด
4 สัปดาห์หลังการผ่าตัด
หากสามารถทานอาหารอ่อนได้ดี สามารถเริ่มทดแทนด้วยอาหารธรรมดาที่มีเนื้อหยาบข้นตามลำดับ แต่ถ้ายังมีอาการคลื่นไส้ ยังไม่สามารถรับประทานอาหารในระยะนี้ได้ ก็ยังสามารถรับประทานอาหารในระยะที่ 3 ต่อไปได้ หรือรับประทานระยะที่ 4 แล้วเกิดคลื่นไส้ ก็สามารถกลับไปรับประทานระยะที่ 3 ก็ได้เช่นกัน เนื่องจากผู้ป่วยไม่จำเป็นต้องเข้าในระยะที่ 4 ตามกำหนดที่แนะนำตามเวลา แต่ขึ้นอยู่กับความพร้อมของผู้ป่วยเป็นสำคัญ ควรเป็นอาหารธรรมดาที่ปรุงสุก โดยเน้นโปรตีนสูงเป็นหลัก สามารถเริ่มรับประทานผักนิ่มๆ ได้ ผลไม้ควรเริ่มทานเป็นผลไม้ปอกเปลือกในปริมาณน้อย ๆ
-
ไก่/หมูอบซอส
-
สเต๊กปลา
-
ลาบหมู หรือไก่ แบบไม่เผ็ด
-
ไข่ยัดไส้
1 เดือนหลังผ่าตัดกระเพาะ
โดยส่วนใหญ่แล้วจะสามารถทานอาหารได้ตามปกติ แต่ควรเลือกทานอาหารเพื่อสุขภาพอาหารที่มีโปรตีนสูง ไม่มัน ไม่ใส่น้ำตาล หรือหวานน้อย และควรเคี้ยวอาหารให้ละเอียดอย่างช้าๆ สำหรับผัก และผลไม้สามารถทานได้ตามปกติ เพื่อควบคุมพลังงานส่วนเกิน และน้ำหนักตัว อาจจะรับประทานวิตามิน และแร่ธาตุเสริมตามคำแนะนำของแพทย์
รีวิวการผ่าตัดศัลยกรรมกระเพาะอาหาร
สาระน่ารู้: การผ่าตัดกระเพาะ / การผ่าตัดรักษาโรคอ้วน
หลังผ่าตัดกระเพาะ ต้องเตรียมตัว เรื่องอาหารอย่างไร?
การผ่าตัดกระเพาะเป็น การผ่าตัดที่ทำให้กระเพาะเล็กลง คนไข้จึงรับประทานอาหารได้น้อยลง ทำให้น้ำหนักลดลง เพื่อป้องกันการขาดสารอาหารที่จำเป็นต่อร่างกายเราต้อง..
ผ่าตัดเอาเนื้อกระเพาะอาหารออก ต่างจาก ทำบายพาสกระเพาะอาหาร อย่างไร
การผ่าตัดกระเพาะอาหารเพื่อลดน้ำหนักมีหลายวิธี สำหรับคนที่ต้องการลดน้ำหนัก อย่างรวดเร็ว การผ่าตัดกระเพาะอาหารแบบ Sleeve Gastrectomy และ Gastric Bypass:
ความเสี่ยงและภาวะแทรกซ้อนจากการผ่าตัดกระเพาะอาหาร
การผ่าตัดกระเพาะแบบ Sleeve gastrectomy เป็นการผ่าตัดลดน้ำหนักที่ได้รับความนิยมมากที่สุด โดยทำให้กระเพาะอาหารเล็กลงและทำให้รับประทานอาหารได้น้อยลง
คำถามที่พบบ่อย
1. หากผ่าตัดกระเพาะอาหาร สามารถกลับมาอ้วนได้อีกหรือไม่ ?
การผ่าตัดกระเพาะ ตามปกติแล้ว โอกาสที่จะกลับมาอ้วนอีกน้อยมาก เพราะ รับประทานอาหารได้น้อยลง ปริมาณกระเพาะเล็กลง แต่ถ้าน้ำหนักลดลงแล้ว แต่ กลับมาอ้วนขึ้นอีก ต้องตรวจหาสาเหตุโรคที่อาจจะเกิดขึ้นได้เช่น Gut Hormone ทำให้ หิวบ่อยขึ้น ไม่รู้สึกอิ่ม
2. การผ่าตัดกระเพาะอาหาร ได้ผลจริงหรือไม่ ?
การผ่าตัดกระเพาะอาหาร ช่วยลดน้ำหนักได้จริง ในระยะแรกน้ำหนักจะลดเยอะมาก ต่อมาจะลดเป็นสัดส่วนที่น้อยลง น้ำหนักจะคงที่ภายใน 1-2 ปีหลังผ่าตัด แต่ควรเป็นทางเลือกสุดท้ายของการลดน้ำหนัก
มีความเสี่ยงเนื่องจากเป็นการผ่าตัดเอาเนื้อกระเพาะออก ไม่สามารถเอากลับคืนมาได้ระยะยาวมีความเสี่ยงกับการขาดวิตามิน เพราะ กระเพาะอาหารสร้างวิตามินบางชนิด
มีความเสี่ยงจากการผ่าตัดเช่น ยาสลบ แผลเย็บไม่ติด ขึ้นกับความชำนาญของแพทย์ผู้ผ่าตัด
ทำไมต้องผ่าตัดกระเพาะอาหารที่โรงพยาบาลศัลยกรรมตกแต่งกมล
- ทีมแพทย์ที่มีประสบการณ์และมีความชำนาญสูงเฉพาะ
- มีทีมดูแลรักษา ก่อนและหลังการผ่าตัดกระเพาะ
- มีเครื่องมือผ่าตัดด้วยกล้อง ที่ทันสมัย มีทีมที่มีประสบการณ์ช่วยการผ่าตัดสูง
- ห้องผ่าตัดทันสมัย เพียบพร้อม
- ห้องพักผู้ป่วยเป็นส่วนตัว สะดวก สบาย สะอาด
- โรงพยาบาล มาตรฐาน ระดับสากล JCI

















