Gender Reassignment Surgery
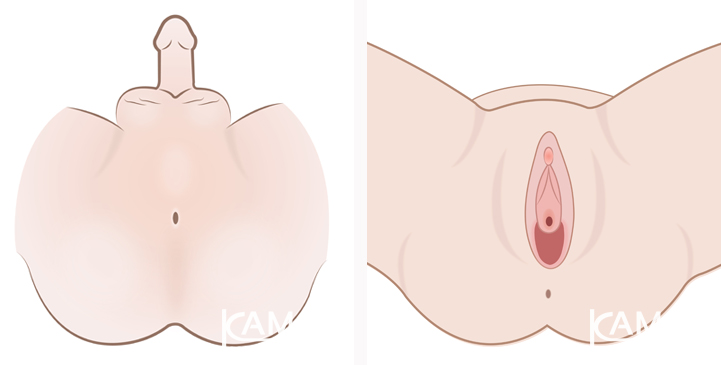
Also known as gender affirmation surgery, or sex reassignment surgery (SRS), is a significant procedure sought by individuals who experience a mismatch between their assigned sex at birth and their inner gender identity.
This incongruence, medically termed Gender Dysphoria, can cause significant distress and impact an individual's quality of life.
Gender reassignment surgery aims to alleviate this distress by aligning one's physical appearance with their true gender identity.
While hormone therapy and other procedures like breast augmentation or voice surgery play a role in the transition journey, gender reassignment surgery is often considered the most impactful step, as it directly addresses the core of gender identity.
It's important to understand that gender reassignment surgery is a deeply personal decision. It's crucial to gather comprehensive information and carefully consider the implications before embarking on this path. This page aims to provide you with a detailed understanding of the procedure, its benefits, and potential considerations.
The Importance of Choosing a Qualified Surgeon for Sex Reassignment Surgery
Gender reassignment surgery is a complex and delicate procedure that demands a high level of skill and expertise from the surgeon.
The surgeon's experience and proficiency significantly influence the outcome of the surgery. A skilled surgeon can ensure that the newly constructed genitalia not only look natural and aesthetically pleasing but also function optimally. This includes creating a vagina with adequate depth for comfortable intercourse and preserving the necessary nerves to allow for sexual sensation and pleasure.
Choosing a qualified and experienced surgeon is paramount to achieving a successful outcome and ensuring a positive surgical experience. A surgeon who specializes in gender reassignment surgery will have a deep understanding of the unique needs and concerns of transgender individuals. They will be able to tailor the procedure to your specific anatomy and goals, ensuring the best possible results.
Why Choose Dr. Kamol for Gender Reassignment Surgery?

Dr. Kamol Pansrithum is a world-renowned expert in gender reassignment surgery, with over 25 years of experience and a remarkable track record of successful procedures. Since 1997, he has performed over 10,000 cosmetic and gender affirmation surgeries, including more than 5,000 male-to-female procedures. His extensive experience and dedication to the field have earned him global recognition as a leader in gender reassignment surgery.
Dr. Kamol is committed to providing the highest quality care and achieving the best possible outcomes for his patients. He continually refines and develops innovative surgical techniques to ensure that his patients receive the most advanced and effective treatment. His methods prioritize natural-looking results, preservation of sexual sensation, optimal vaginal depth, and minimal scarring.
Beyond his surgical expertise, Dr. Kamol is a respected figure in the medical community. He has been invited to share his knowledge and experience as a speaker at numerous international medical institutions. He has also authored and contributed to academic articles published in leading medical journals, further solidifying his position as a thought leader in the field of gender reassignment surgery.
See more of Dr. Kamol's Profile
Goals of Gender Affirmation Surgery at Kamol Cosmetic Hospital
At Kamol Hospital, we believe in a patient-centered approach to gender reassignment surgery. We understand that each individual has unique needs and desires, and we strive to tailor our procedures to achieve the best possible outcome for each patient. Our surgical approach is guided by the following key goals:
- Create Genitalia that Resembles a Woman as Closely as Possible: We aim to create a natural-looking and aesthetically pleasing result that harmonizes with the individual's body and enhances their sense of femininity.
- Maximize Vaginal Depth: We strive to create a vagina that is as deep as possible, taking into account the patient's individual anatomy and tissue availability. This ensures comfortable and satisfying sexual intercourse.
- Preserve Sexual Sensation: We prioritize the preservation of nerves to ensure the ability to experience sexual pleasure and achieve orgasm after surgery.
- Minimize Scarring: Our surgical techniques are meticulously designed to minimize the visibility of scars, promoting a natural and aesthetically pleasing outcome.
Dr. Kamol's Surgical Technique for Sexual Arousal
Dr. Kamol recognizes the importance of sexual well-being after gender reassignment surgery. He has developed specialized surgical techniques to optimize sexual sensation and pleasure for his patients. These techniques involve carefully dissecting and repositioning the nerves from the penis to various locations within the newly created genitalia. This creates multiple points of sensitivity, enhancing the potential for sexual arousal and orgasm after surgery.
-
- Sensory point 1: Nerve number 1 from the penis is taken to form the clitoris (as shown in Figure 1).
- Sensory point 2: Take nerve number 1 and implant it under the inner cam.
- Sensory point 3: Nerve implants are placed beneath the urethra on both the left and right sides.
- Sensory point 4: Cowper's glands or Bulbourethral glands, which are located in front of the prostate gland, are nerve-filled glands that produce lubricant, so during intercourse, there will be lubrication and sexual sensation at this location. We keep this gland and bury it near the urethra [1].
- Sensory point 5: The G spot, which is the sensory spot located beneath the prostate gland. We make the vagina as deep as possible, approaching the prostate gland and the G spot [2].
- Some surgeons claim to be the only ones in the world who can treat the sexual nerves. This is not true at all.
- The location of the sensory points at the tip of the penis will be made and implanted at various parts of the newly created female genitalia (as shown in Figure 1).
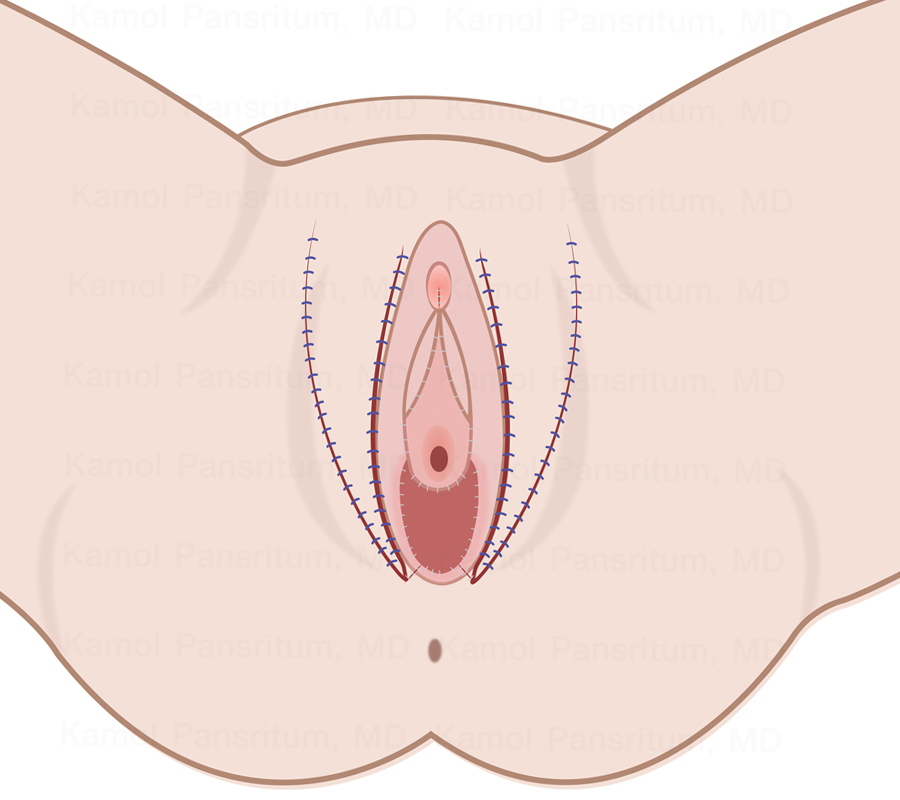
- Dr. Kamol Pansrithum has developed a new technique that causes the least amount of scarring (as shown in Figure 2) compared to the previous technique (as shown in Figure 3).
Sexual function and sensation by Dr. Kamol's techniques.
- Background: The nerve ending to the clitoris and the glans penis are similar, with approximately 8,000 nerve endings.
- Dr. Kamol technique uses surgical techniques to identify and preserve all the nerves from glans penis precisely and creates 4 points of special
sexual arousal as follows:
a.The first point is the neo-clitoris.
b.The second area, located at the inner sides of the labia minora, contains the additional nerve ending from the nerve trunk.
c.The third point is the bilateral ridge of the neo-urethral plate that Dr. Kamol creates from the skirt of the glans penis containing the nerve ending.
d.The fourth spot is at the bulbourethral glands before the prostate glands. Dr. Kamol always keeps the bulbourethral glands containing the nerve ending and mucous secretion.1
e.The fifth spot (G-spot) is at the lower part of the prostate glands and consists of sensory nerve endings. Dr. Kamol creates the neo-vagina very close to the surface of the prostate glands.2 - Some surgeons claim their technique is the only one (in the world) that preserves the erotic nerve ending to the neo-vagina, but this is not true.
- Schematic of the glans penis and the areas are moved to reconstruct the neo vagina (Figure 1)
- Dr. Kamol creates a minimal-short scar comparison to other conventional techniques (Figure 2).
The area from the head of the penis to the neovagina.
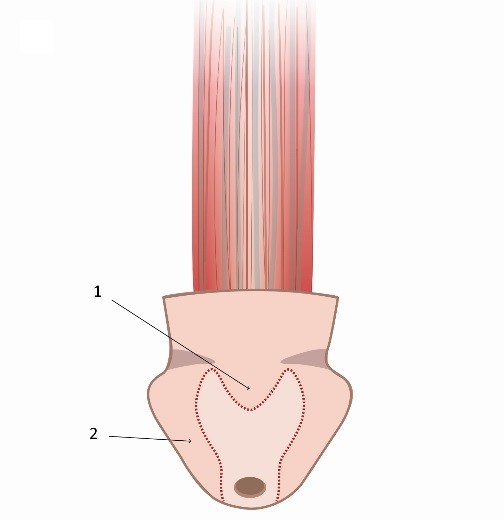
Figure 1. The areas of the head of the penis form the neovagina.
- The tip of the head of the penis forms the neoclitoris (1),
- The skirt of the head of the penis creates the sensation of the second point (2).
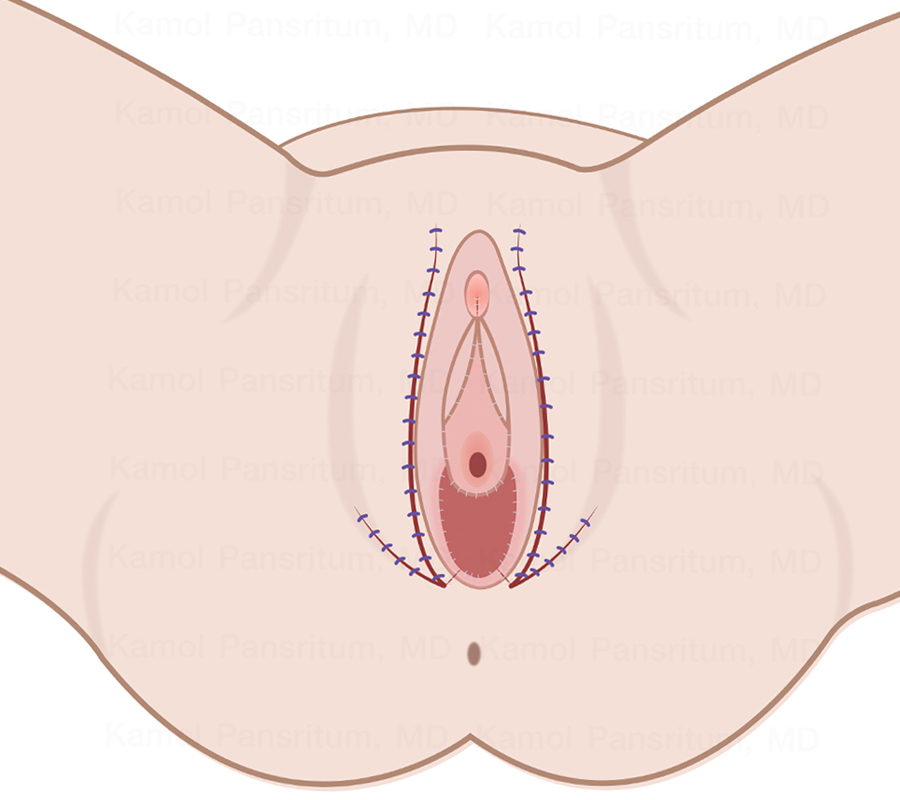
Figure 2. Dr. Kamol's technique (short scar)
Figure 3. Other techniques (long scar)
Qualifications for Gender Transition Surgery
Gender reassignment surgery is a major life decision, and it's important to ensure that individuals are fully prepared for the procedure and its implications. At Kamol Cosmetic Hospital, we adhere to strict guidelines to ensure the safety and well-being of our patients. Individuals considering male-to-female gender reassignment surgery should meet the following criteria:
- Age: Be at least 20 years old. If under 20, parental or guardian consent is required.
- Hormone Therapy: Have undergone continuous hormone therapy for at least one year. This helps prepare the body for surgery and promotes the development of feminine characteristics.
- Gender Identity: Have a long-standing and consistent gender identity as female. This means that you have consistently identified as female for a significant period.
- Living as Female: Have lived as a woman for at least one year. This demonstrates a commitment to living in your true gender role.
- Gender Dysphoria: Experience significant distress due to gender dysphoria. This indicates that the mismatch between your assigned sex and gender identity is causing significant emotional and psychological discomfort.
- Mental Health Assessment: Have undergone a mental health assessment and received a certificate from a psychiatrist confirming their suitability for surgery. This ensures that you are mentally and emotionally prepared for the procedure and its implications.
- Physical Health: Be in good overall health. This minimizes the risks associated with surgery and promotes a smooth recovery.
The Importance of Psychological Assessment Before Sex Change Surgery
A comprehensive psychological assessment is an essential component of the pre-operative process for gender reassignment surgery. This assessment serves several important purposes:
- Assessing Readiness: It helps determine whether the individual is fully prepared for the procedure and its potential impact on their life.
- Identifying Mental Health Concerns: It helps identify any underlying mental health conditions that may affect their decision-making or post-operative adjustment.
- Evaluating Understanding and Expectations: It assesses their understanding of the surgery, their expectations for the outcome, and their plans for the future.
- Providing Support: It provides an opportunity for individuals to discuss their concerns and receive support from a mental health professional.
5 Techniques for Male-to-Female Sex Reassignment Surgery at Kamol Hospital
Kamol Hospital offers a range of surgical techniques for male-to-female gender reassignment. Each technique has its own advantages and considerations, and the most suitable option will depend on individual anatomy, preferences, and surgical goals.
Technique 1: Vaginoplasty without Depth
This technique focuses primarily on constructing the external female genitalia, including the labia majora, labia minora, clitoris, and urethral opening.
It does not create a deep vaginal canal. This option may be suitable for individuals who do not prioritize penetrative intercourse.
Pros: Ideal for those with no interest in vaginal penetration.
Cons: Does not create a deep vaginal canal.
Technique 2: Creating a Vagina Using Skin from the Penis (Skin Inversion Technique)
This is one of the most common techniques used in male-to-female gender reassignment surgery. It involves using the skin of the penis to create the lining of the vagina. The skin is carefully inverted and sutured to form the vaginal canal.
This technique is relatively straightforward and has a shorter operating time compared to some other methods.
However, the depth of the vagina achieved with this technique may be limited, especially for individuals with shorter penises.
Pros: Straightforward procedure (approx. 4 hours) and shorter recovery time.
Cons: Unsuitable for those with a penis under 4 inches in length.
Technique 3: Vaginal Creation Technique Using Skin from the Penis and Skin from the Testicles (Scrotal Skin Grafting Technique)
This technique combines skin from both the penis and the scrotum to create a deeper vaginal canal. The skin from the scrotum is thinned and grafted onto the penile skin, increasing the overall surface area available for vaginal construction.
This method offers the potential for greater vaginal depth compared to the skin inversion technique. However, it is a more complex procedure with a longer operating time.
Pros: Can help individuals with smaller penises achieve a vaginal depth of 6+ inches.
Cons: The surgery is more complicated (approx. 6 hours) and thus a greater margin for error. Longer recovery time.
Technique 4: Creating a Vagina Using the Colon to Make the Vaginal Wall (Colon Vaginoplasty Technique)
This technique involves using a section of the colon to create the lining of the vagina. The colon is naturally lubricated, which can be an advantage for some individuals.
Colon vaginoplasty can provide excellent vaginal depth and a more natural feel. However, it is a more extensive surgery with a longer operating time and recovery period.
Kamol Cosmetic Hospital offers two approaches to colon vaginoplasty:
- Open Colon Vaginoplasty: This traditional approach involves an incision along the bikini line to access the colon.
- Laparoscopic Colon Vaginoplasty: This minimally invasive approach uses small incisions and specialized instruments, resulting in less scarring and potentially faster recovery.
Pros:
- This method helps patients who have previously undergone gender reassignment surgery and who require a deeper vaginal canal.
- This method can be used in patients with very short penis.
- The vagina contains natural lubrication.
- The depth of the newly created vagina can be determined in advance. This method provided the deepest vaginal canal of all methods.
- This method provides a very strong and elastic vaginal canal and does not require lifelong dilation.
- This is a well-studied method that has been used for many years.
- Contrary to rumors, the sigmoid colon vagina is odorless. Less than 4% may experience an unpleasant odor, and this can be eliminated with improved hygiene.
Cons:
- Scarring (7-10 cm) above the left pubic bone.
- The surgery is more complicated and the colon must be cleansed with an enema in advance.
- Patients may experience bloating for 2 to 3 days after surgery.
- Unsuitable for individuals who are overweight. The BMI should not exceed 27.
- Cannot be performed on individuals with a history of chronic colitis or Crohn's disease.
Technique 5: Creating a Vagina Using the Abdominal Wall and Skin from the Penis (Penile-Peritoneal Vaginoplasty: PPV)
This innovative technique combines skin from the penis with the peritoneal lining of the abdomen to create the vagina. The peritoneum is a thin, moist membrane that lines the abdominal cavity.
This technique offers good vaginal depth and natural lubrication. However, it may not be suitable for all individuals, particularly those with a history of abdominal surgery or certain medical conditions.
Pros:
- The vagina contains natural lubricant without an unpleasant odor.
- The vagina is elastic and stretchable, like a biological vagina.
- The chance of vaginal prolapse and shrinkage is less compared to all other types of SRS.
- The vagina is elastic and the dilation may decrease within a year.
- Natural lubrication is similar to vaginal lubrication.
- Recovery is fast and there are fewer risks compared to sigmoid colon.
- Peritoneal stretching (Davydov's method) has been performed on cisgender girls for over 40 years and has been well-studied.
Cons:
- Unsuitable for those with short penises.
- Patients may experience bloating for 2 to 3 days after surgery.
- Unsuitable for individuals who are overweight.
- 1 year after surgery, if there is a problem with the junction between the skin and the abdominal wall, a new vaginal revision surgery may be required.
- A chance for visible scarring.
- The surgery is more complex (4 to 6 hours).
Why is Body Mass Index (BMI) and Weight important for SRS?
The risks of surgery are increased by obesity. Obesity can create additional challenges in surgery, it can increase the risk of complications such as infection, blood clotting, surgical failure, delayed wound healing and breathing problems. Optimal weight and BMI can reduce risks and complications. Excess weight combined with other factors including aging and medical conditions increases the likelihood of postoperative complications. The patient should provide the doctor with all medical information before scheduling surgery.
Accepted for surgery in case of:
- SRS- PPV penile-peritoneal vaginoplasty BMI less than 30 and Weight less than 90 kg.
- SRS- Laparoscopic Sigmoid Vaginoplasty Technique BMI less than 30 and Weight less than 90 kg.
- SRS- Vaginoplasty with scrotal skin grafting BMI less than 30 and Weight less than 90 kg.
- SRS - Open Sigmoid Vaginoplasty BMI less than 26 and Weight less than 80 kg.
Removal of Genital Hair Before Sex Reassignment Surgery
The extent of genital hair removal required before surgery varies depending on the chosen surgical technique and individual anatomy. Your surgeon will provide specific instructions regarding hair removal. In general, hair removal may be necessary in the areas where the skin will be used for vaginal construction.
We recommend:
- SRS without a vaginal cavity, this procedure does not need to do genital hair removal.
- SRS skin inversion: this technique requires genital hair removal in areas 1,2,3 in picture 1.
- SRS skin graft technique needs to remove the hair at around 5x6 cm at the base of the penis, as in picture 1.
- SRS with colon graft, we need the patient removes the hair at the vaginal entrance at around 5x6 cm at the base of the penis as in picture 1.
- SRS-PPV, the patient needs to remove the hair in areas of 1,2,3 in picture 1.

Picture 1. Shows the area of the hair removal
Methods of Male-to-Female Sex Change Surgery: A Step-by-Step Overview
While the specific surgical techniques may vary, the general steps involved in male-to-female gender reassignment surgery include:
- Anesthesia: The surgery is performed under general anesthesia administered by a qualified anesthesiologist to ensure your comfort and safety throughout the procedure.
- Creating a New Vagina: A space is created between the rectum and urethra to accommodate the new vagina. The depth and width of this space will depend on the chosen surgical technique and individual anatomy.
- Taking Skin from the Original Penis or Testicles: The skin from the penis and/or scrotum is carefully harvested and prepared for use in constructing the vaginal lining and external genitalia.
- Preserving the Sexual Nerves: The nerves responsible for sexual sensation are meticulously identified and preserved. These nerves will be used to create the clitoris, ensuring the potential for sexual pleasure after surgery.
- Cutting the Male Urethra: The urethra is shortened and repositioned to allow for proper urination from the newly created vaginal opening.
- Reshaping the External Areas: The labia majora, labia minora, urethra, and clitoris are carefully sculpted and positioned to create a natural-looking and aesthetically pleasing female genitalia.
Preparation Before Male-to-Female SRS
Proper preparation is crucial for a successful surgery and smooth recovery. Here are some key steps to take before your gender reassignment surgery:
- See a Psychiatrist: Obtain a mental health assessment and certificate from a qualified psychiatrist. This confirms that you are mentally and emotionally prepared for the procedure and its implications.
- Consult a Surgeon: Schedule a consultation with your surgeon to discuss the procedure in detail, undergo a physical examination, and review your medical history. You may also need to undergo tests such as a chest X-ray, blood tests, EKG, and stress test, especially if you are over 40 years old.
- Stop Hormones: Discontinue hormone therapy for 1-2 weeks before surgery, as advised by your doctor. This helps stabilize your hormone levels and minimize potential complications.
- Stop Medications: Avoid medications that can affect blood clotting, such as aspirin, anti-inflammatory drugs, or certain herbal supplements, for at least 2 weeks before surgery. Your doctor will provide specific guidance on which medications to avoid.
- Stop Smoking: Refrain from smoking for at least 2 weeks before and after surgery. Smoking can impair wound healing and increase the risk of complications.
- Prepare for Recovery: Make arrangements for post-operative care, including assistance with daily tasks, wound care, and transportation to follow-up appointments.
Post-operative wound Care for Non-Intestinal SRS
After your gender reassignment surgery, you will need to follow specific post-operative care instructions to ensure proper healing and minimize complications. Here are some general guidelines for non-intestinal gender reassignment surgery:
- Hospital Stay: You will typically stay in the hospital for 4-6 nights for close monitoring and wound care. The medical staff will provide pain medication, assist with hygiene, and monitor your vital signs.
- Dietary Restrictions: You may need to follow dietary restrictions, especially in the first few days after surgery.
- Positioning: You will be advised on proper positioning to minimize swelling and promote healing. This may involve lying on your back with your hips elevated.
- Wound Care: Keep the surgical area clean and dry. Attend follow-up appointments for wound checks and dressing changes. Your surgeon will provide specific instructions on how to care for your wound.
- Catheter Care: If you have a urinary catheter, follow the instructions provided for proper care and hygiene.
- Vaginal Dilation: You may need to use a dilator to maintain the depth and width of the vagina, as instructed by your surgeon. This helps prevent narrowing or stenosis of the vagina.
- Activity Restrictions: Avoid strenuous activity and sexual intercourse for at least 2 months to allow for proper healing.
- Follow-up Appointments: Attend regular follow-up appointments with your surgeon to monitor your progress and address any concerns.
- Day 1 & 2: For the first two days after surgery, you should avoid foods and drinks containing fiber, such as fruit juices, milk and yogurt, as they will cause waste to be released. This may lead to contamination of the wound.
- Day 1 & 2: For the first one or two days after surgery, you will be required to lie on your back with your hips raised with your legs slightly apart, as this will help reduce swelling.
- Day 3: On the third day after the operation, you can lie on your side.
- Day 3: On the third day after surgery, your surgeon will remove the drainage tube, open and dress the wound. Anyone who has undergone sex reassignment surgery with skin grafts or sex reassignment surgery with colon transplants must remain in bed for up to six days until the urinary catheter is removed.
- Day 6: On the sixth day after surgery, patients who have undergone gender reassignment surgery with skin grafting will have their urinary catheter removed. The wound will be bandaged and you can be transferred to a special apartment for further recovery.
Post-operative wound Care for Intestinal SRS
If you have undergone colon vaginoplasty, which involves using a section of the colon to create the vaginal lining, you will have additional post-operative care instructions:
- Bowel Rest: You may need to refrain from eating or drinking anything until your bowel function returns to normal. This allows the colon to rest and heal.
- Gradual Diet Progression: Once your bowel function resumes, you will start with clear liquids and gradually progress to solid foods as tolerated. This helps prevent nausea, vomiting, and bloating.
- Close Monitoring: Your bowel function and overall recovery will be closely monitored by the medical staff.
In addition to the above, the following post-operative care instructions apply to both non-intestinal and intestinal gender reassignment surgery:
- Catheter Care: If you have a urinary catheter, follow the instructions provided for proper care and hygiene.
- Vaginal Dilation: You will likely need to use a dilator to maintain the depth and width of the vagina, as instructed by your surgeon. This helps prevent narrowing or stenosis of the vagina.
- Activity Restrictions: Avoid strenuous activity and sexual intercourse for at least 2 months to allow for proper healing. The patient can engage in light activity after three weeks and can resume regular daily activities after 3 months.
- Follow-up Appointments: Attend regular follow-up appointments with your surgeon to monitor your progress and address any concerns.
- Day 1 - 3: For the first three days, you must not eat or drink until bowel function is restored. During this period, you will receive intravenous fluids.
- Month 1: The patient should avoid heavy meals during the first month.
Possible Risks and Complications of SRS
While gender reassignment surgery is generally safe, it's essential to be aware of the potential risks and complications. These can include:
- Swelling, Bruising, and Hematoma: These are common after any surgery and usually subside with time.
- Bleeding, Infection: These complications can occur but are minimized with proper surgical technique and post-operative care.
- Recto-Vaginal Fistula: This is an abnormal connection between the rectum and vagina, which may require further surgery to correct.
- Poor Wound Healing and flap Necrosis: These complications can occur but are less common with proper wound care and adherence to post-operative instructions.
- Vaginal and Urethral Stenosis: Narrowing of the vagina or urethra may occur and can be addressed with dilation or further procedures if necessary.
- Unsatisfied Size or Shape: While surgeons strive for optimal results, the final size and shape of the genitalia may vary. It's important to have realistic expectations and discuss your goals with your surgeon.
- Wound Pain: Pain is expected after surgery and can be managed with medication.
- Asymmetric Labia: The labia may not be perfectly symmetrical, which is often a normal variation.
- Scarring: Scarring is inevitable with any surgery, but surgical techniques aim to minimize its visibility.
- Decreased Sensation: Some decrease in sensation may occur, but nerve-sparing techniques are used to preserve as much sensation as possible.
- Deep Vein Thrombosis: Patients with a history of blood clotting disorders are at increased risk and should inform their doctor. Preventive measures, such as compression stockings or medication, may be recommended.
- Anesthesia Side Effects: All surgeries carry risks associated with anesthesia, such as nausea, vomiting, or allergic reactions.
Why Choose Kamol Cosmetic Hospital for Sex Affirmation Surgery?
Kamol Hospital is a leading provider of sex reassignment surgery, and we are dedicated to providing our patients with the highest quality care and support. Here's why you should consider choosing us for your gender affirmation journey:
- Experienced Surgeons: Our surgical team comprises highly skilled and experienced surgeons who specialize in gender reassignment procedures. They have a deep understanding of transgender healthcare and are committed to achieving the best possible outcomes for their patients.
- Innovative Techniques: We utilize the latest surgical techniques and technologies to ensure optimal results, minimize complications, and promote a smooth recovery.
- Comprehensive Care: We provide comprehensive care that addresses both the physical and emotional aspects of gender transition. Our team includes not only surgeons but also nurses, counselors, and support staff who are dedicated to your well-being throughout your journey.
- State-of-the-Art Facilities: Our hospital is equipped with modern facilities and state-of-the-art equipment to ensure patient safety and comfort.
- Affordable Prices: We offer competitive prices for our high-quality services, making gender reassignment surgery more accessible to individuals seeking care.
- International Patient Support: We cater to international patients with dedicated support staff who can assist with travel arrangements, accommodation, and language interpretation.
We understand that gender reassignment surgery is a significant step, and we are committed to providing you with the support and care you need to achieve your gender goals and live authentically. If you have any questions or would like to schedule a consultation, please don't hesitate to contact us.
Getting to Know for Gender Reassignment Surgery
Why Colon Vaginoplasty needs Rejuvination
Colon Vaginoplasty rejuvenation is a procedure that aims to improve the health and function of the colon tissue used in..
Vaginoplasty for MRKH, Congenital Birth Defect.
Vaginoplasty is a surgical procedure that is used to reconstruct or repair the vagina. In some cases, it may be used to treat..
Dilation keeps Neo-vagina cavity
A vagina created through surgery, typically requires vaginal cavity dilation in order to maintain its size and function.
Please take a look at the results of vaginoplasty.
Video : Our testimonials for Gender Reassignment Surgery
Frequently Asked Questions (FAQs)
A: Sex Reassignment Surgery (SRS), also known as Gender Confirmation Surgery (GCS) or Gender Affirming Surgery (GAS), encompasses a range of surgical procedures designed to align an individual's physical appearance with their gender identity. These procedures may involve altering primary and/or secondary sexual characteristics.
A: We offer a comprehensive range of SRS procedures, including:
Male-to-Female (MTF) Surgeries:
- Facial feminization surgery
- Breast augmentation
- Orchiectomy (removal of testicles)
- Vaginoplasty (creation of a vagina)
Female-to-Male (FTM) Surgeries:
- Masculinizing chest surgery (top surgery)
- Hysterectomy (removal of the uterus)
- Oophorectomy (removal of the ovaries)
- Metoidioplasty or phalloplasty (construction of a penis)
A: Eligibility is determined through a comprehensive assessment process, which typically includes:
- Mental health evaluations: To ensure you're mentally prepared for the surgery and its implications.
- Hormone therapy: A period of hormone therapy may be required to align your physical characteristics with your gender identity.
- Real-life experience: Living in your desired gender role for a specified period may be necessary to demonstrate your commitment to the transition.
Our team will guide you through the eligibility criteria and assessment process, ensuring you have all the information you need to make an informed decision.
A: Recovery time varies depending on the specific procedure(s) performed. Generally, you can expect to stay in the hospital for a few days to a week following surgery, with full recovery taking several weeks to months. We provide detailed aftercare instructions and support to ensure a smooth and comfortable recovery.
A: As with any surgical procedure, gender affirmation carries potential risks and complications, including:
- Infection
- Bleeding
- Scarring
- Nerve damage
- Complications with anesthesia
Our experienced surgical team takes every precaution to minimize these risks and ensure your safety and well-being.
A: The cost varies depending on the specific procedures involved. We offer competitive pricing and transparent cost structures. During your consultation, we'll provide a personalized quote and discuss financing options.
A: Our surgeons are board-certified plastic surgeons with specialized training and extensive experience in performing Gender Affirmation Surgery. They are committed to providing the highest quality care and achieving the best possible outcomes for our patients.
A: The process typically involves the following steps:
- Initial Consultation: You'll meet with our surgical team to discuss your goals, undergo a physical examination, and review your medical history.
- Assessment and Preparation: We'll conduct a comprehensive assessment to determine your eligibility for surgery and provide you with detailed pre-operative instructions.
- Surgery: Our experienced surgical team will perform the surgical procedure(s) in our state-of-the-art facilities.
- Post-Operative Care: You'll receive comprehensive aftercare instructions and support to ensure a smooth and comfortable recovery.
- Follow-Up Appointments: We'll schedule follow-up appointments to monitor your progress and address any concerns you may have.
A: We understand that undergoing SRS is a significant decision, and we're committed to providing comprehensive support throughout your journey. Our team offers:
- Pre-operative counseling and education
- Assistance with travel and accommodation for some procedures
- Personalised aftercare and support
- Ongoing follow-up care
A: We encourage you to schedule a consultation with our surgical team to discuss your individual needs and goals. We'll provide you with detailed information about the different procedures available, the potential risks and benefits, and the recovery process. We'll also answer any questions you may have and help you make an informed decision.
A: You cancontact usthrough our website, email, or phone. Our friendly and knowledgeable staff will be happy to assist you and answer any questions you may have.